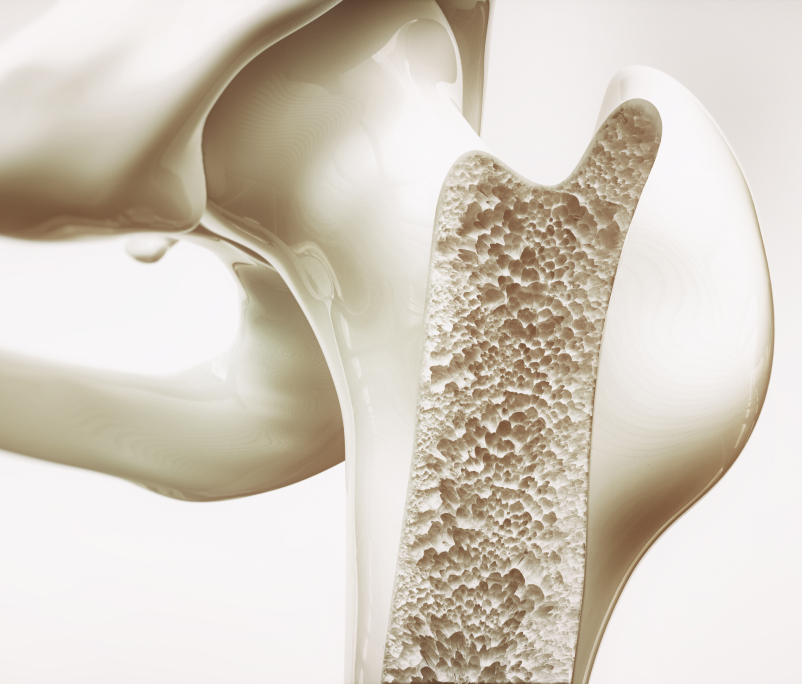
Understanding the Multifaceted Nature of Bone Health
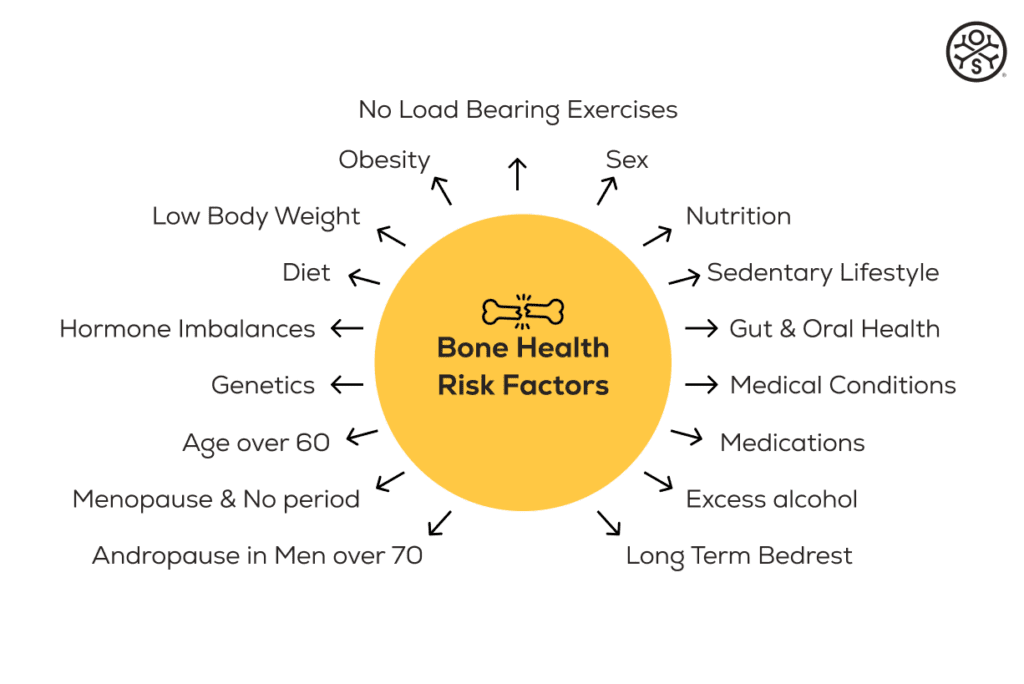
Bone health is crucial for overall well-being, yet it’s often compromised by various factors. Understanding these can be key in prevention and management.
Age is a major contributor, as bones lose density and strength naturally over time. Hormonal changes, especially in women during and after menopause due to a decrease in estrogen, significantly affect bone density.
Nutritional deficiencies are also key, particularly insufficient intake of vitamins, minerals, protein and healthy fats for bone and muscle formation and maintenance.
Lifestyle choices such as a lack of physical activity, excessive alcohol use, and smoking can exacerbate bone weakening. Certain medications, like long-term corticosteroids, and medical conditions including thyroid disorders and celiac disease, can negatively impact bone health. Genetic predisposition also plays a role, with a family history of osteoporosis indicating higher risk. Therefore, a combination of genetic, lifestyle, and environmental factors contributes to poor bone health, and addressing these can help in its prevention and management.
Below is a discussion about the main causes and risk factors associated with Bone Health.
Genetics – The Hereditary Factor
Poor bone health can be hereditary, check if any relative has been diagnosed. Parents and sibling that have broken bones from minor falls or rapidly lost height can indicate an increased risk of poor bone health.
However, recent scientific findings indicate that genetics account for less than 20% of our overall health, while epigenetic factors, such as modifiable lifestyle, nutritional, and environmental elements, contribute to over 80% of our bone, muscle, and metabolic health.
Therefore, familial osteoporosis is more likely attributed to a combination of factors rather than genetics alone.
Nutritional – Building Blocks of Bone and Muscle Health
It is important to recognise that the standard health authority specified RDA’s (Recommended Daily Allowances) for vitamins, minerals, protein, and healthy fats, are only minimums to avoid acute deficiencies.
The levels recommended are not optimal to enable you to feel or perform your best or to treat a disease process. They are also not appropriate for someone with osteoporosis needing to rebuild bone, or for an athlete wanting to build bigger, stronger, muscles.
If you already have poor bone or muscle health, relying solely on RDA’s, which are designed to prevent chronic disease, or the old Food Pyramid Guide for the 90’s, will most likely not be adequate.
Instead, a focused approach on increasing the intake of vitamins, minerals, protein, and healthy fats essential for bone and muscle repair is necessary.
Experts now recognise that no single diet, including Mediterranean, vegan, vegetarian, paleo, keto, low FODMAP, Atkins, flexitarian, or carnivore, is nutritionally sufficient for people with poor bone and muscle health including osteoporosis of sarcopenia, especially given today’s lower nutrient density in foods.
In addition, restrictive diets or those low in macro vitamins D, B, and Calcium can increase the risk of developing low bone density. Other important nutrients include vitamins A, E, B’s including Folate B9, K, C, Magnesium, Zinc, Boron, Chromium, Silicon, Omega-3 & Omega-6. Measuring and monitoring these is recommended for people with osteoporosis and addressing deficiencies with diet or supplements, as necessary.
Reversing bone loss and addressing low bone density requires a comprehensive approach, tailored to individual nutritional needs, rather than following a specific popular diet and specialised medical advice is recommended to manage your nutritional requirements.
Complete Amino Acids – Proteins
Diets deficient in essential and complete amino acids, the building blocks of protein necessary for the maintenance and growth of bones and muscles, can result in poor musculoskeletal health. Vegetarian and vegan diets, which often lack complete proteins, need to be carefully managed to ensure they don’t compromise bone and muscle health. It’s important to include whole proteins that meet the Digestible Indispensable Amino Acid Score (DIAAS) criteria in these diets to maintain optimal musculoskeletal health.
Sedentary Lifestyle – A Modern Challenge
Maintaining an active lifestyle up to age 30 is crucial for building optimal bone density which serves as a vital “bone bank” for old age. This period of life is key for providing a robust foundation that helps sustain bone health and resilience as we age. From age 30 the body naturally begins to lose bone density. Physical activity, especially weight-bearing and high impact exercise, such as OsteoStrong® stimulates bone formation. Without this stimulus, bone loses density faster, increasing the risk of low bone health and fractures.
Gut Health – The Nutrient Absorption Factor
Ensuring proper nutrition is vital for bone and muscle health, but if gut and malabsorption conditions hinder the body’s ability to absorb these nutrients, bone and muscle health can be significantly compromised. Such conditions can include:
- Celiac Disease: An autoimmune disorder triggered by gluten that damages the small intestine lining, leading to nutrient malabsorption.
- Crohn’s Disease: A type of inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal tract, impairing nutrient absorption.
- Chronic Pancreatitis: Inflammation of the pancreas that reduces the production of essential enzymes for nutrient digestion and absorption.
- Cystic Fibrosis: A genetic disorder affecting the lungs and digestive system, including the pancreas, leading to poor nutrient absorption.
- Short Bowel Syndrome: A condition resulting from the surgical removal of a significant portion of the small intestine, leading to inadequate nutrient absorption.
- Whipple’s Disease: A rare bacterial infection that can affect the small intestine, impairing nutrient absorption.
- Lactose Intolerance: Inability to digest lactose due to low levels of lactase enzyme, leading to malabsorption of lactose.
- Bile Acid Malabsorption: A condition where the intestines don’t properly absorb bile acids, leading to digestive issues and nutrient malabsorption.
- Gut Dysbiosis: Imbalance of the gut microbiota (bacteria), which can impact nutrient absorption.
- Certain Surgical Procedures: Such as gastric bypass surgery, which alters the digestive system and can affect nutrient absorption.
- Candida: Candida, a fungal infection can cause infections like thrush and candidiasis. In severe instances of systemic candidiasis, it can spread to bones and joints, causing osteomyelitis or septic arthritis, which can lead to pain, swelling, and potential long-term damage.
- Intestinal Parasites: Such as Giardia, which can lead to malabsorption.
- Inflammatory Bowel Diseases (IBD), including Crohn’s Disease and Ulcerative Colitis: Chronic inflammation in the gastrointestinal tract can interfere with the absorption of vital nutrients, leading to deficiencies that weaken bones and muscles.
- Irritable Bowel Syndrome (IBS): While not directly causing malabsorption, IBS can lead to dietary restrictions or changes that might result in insufficient nutrient intake, affecting bone and muscle health.
- Small Intestinal Bacterial Overgrowth (SIBO): This condition can lead to malabsorption of nutrients and subsequent deficiencies that impact bone density and muscle function.
- Lactose Intolerance: Can lead to avoidance of dairy products, potentially resulting in inadequate intake of calcium and vitamin D.
- Bile Acid Malabsorption: This can affect fat absorption and consequently the absorption of fat-soluble vitamins like vitamin D.
Proper diagnosis and management of these conditions, often involving dietary adjustments, prebiotics and probiotics and supplementation, may be necessary crucial for protecting and enhancing musculoskeletal and overall health.
Oral Health – The Gateway to Overall Health
Oral health issues can have a significant impact on bone and muscle health through various mechanisms:
Periodontal Disease (Gum Disease): This condition involves inflammation and infection of the gums, which can lead to the destruction of the jawbone. The chronic inflammation associated with periodontal disease can also contribute to systemic inflammation, potentially affecting overall bone and muscle health.
Tooth Loss and Bone Atrophy: Losing teeth without appropriate dental replacements like implants can lead to the loss of alveolar bone in the jaw. This bone loss can affect the structural integrity of the jaw and overall facial musculature.
Abscesses and Infections: Oral infections, if left untreated, can spread to other parts of the body, potentially affecting the bones and muscles. In severe cases, bacteria from a dental abscess can enter the bloodstream, leading to systemic infections that impact various body systems, including the musculoskeletal system.
Malnutrition Due to Poor Oral Health: Issues like tooth loss, cavities, or oral pain can lead to difficulty in eating, resulting in inadequate nutrition. This can contribute to deficiencies in essential nutrients required for bone and muscle health, such as calcium, vitamin D, and protein.
TMJ Disorders: Problems with the temporomandibular joint (TMJ) can lead to pain and dysfunction in the jaw muscles. This can have a cascading effect on overall posture and muscle alignment, potentially affecting nutrition and bone and muscle health.
Chronic Oral Inflammation: Like periodontal disease, any chronic inflammation in the oral cavity can contribute to systemic inflammation, which has been linked to a range of health issues, including those affecting bones and muscles Lymes.
In recent years research has revealed links between oral health and medical conditions including Endocarditis, Diabetes, Pregnancy Complications, Pneumonia, Jaw Osteoporosis: Alzheimer’s Disease, brain health, Rheumatoid Arthritis, Oral and Throat Cancers, Stroke, Parkinson’s Disease, Cognitive Decline and Vascular Dementia.
The proposed mechanism suggests that oral bacteria, or their toxic byproducts, enter the bloodstream through inflamed or bleeding gums and then travel to other body parts, including the brain. Once in the brain, these bacteria can initiate an immune response or directly inflict damage, potentially leading to cognitive decline or the onset of neurological and other health conditions. Additionally, the inflammation they cause can spread, affecting bone health and overall well-being.
Therefore, maintaining good oral health is important not just for the health of teeth, gums, and jawbone, but also for the overall health.
Regular dental check-ups and good oral hygiene practices are key components of overall health maintenance.
Low Body Weight Challenges
Low body weight is often associated with inadequate nutrition including deficiencies in calcium, protein, vitamins D & K and other nutrients essential for maintaining bone and muscle strength. Being underweight can be associated with hormonal imbalances such as reduced estrogen in women and testosterone in men, leading to bone health issues. Decreased muscle mass is also often associated with poor bone health, because muscles help maintain bone strength. Pre menopause women who stop having their period due to low body weight
Non load bearing exercises
Exercise like endurance swimming and cycling that are non-load bearing, can negatively affect bone density. By incorporating appropriate osteogenic loading like OsteoStrong® into lifestyles, this risk can be reduced.
Age Over 60: The Hormonal Factor
People over 60 years old face an increased risk for osteoporosis, due to hormonal changes that occur with aging. Women experience a decline in estrogen, while men have lower testosterone levels, both of which contribute to decreased bone density. This age-related reduction in bone strength is significant; statistics indicate that 1 in 2 women over 60 and 1 in 3 men over 70 suffer from poor bone health. These figures highlight the importance of proactive bone health management and monitoring in older adults.
Medical Conditions Affecting Bone and Muscle Health
Many medical conditions specifically impact bone and muscle health:
Rheumatoid Arthritis: An autoimmune disorder causing inflammation in joints, which can lead to bone erosion and muscle weakness.
Hyperthyroidism and Hypothyroidism: Thyroid disorders that can affect bone density and muscle strength.
Celiac Disease: An autoimmune disorder where gluten intake leads to damage in the small intestine, affecting nutrient absorption and thus bone and muscle health.
Type 1 and Type 2 Diabetes: Can affect bone density, muscle function, and increase the risk of fractures.
Obesity: A metabolic condition leading to diabetes and many health problems that affect bone and muscle health.
Chronic Kidney Disease: Can lead to changes in bone metabolism and muscle wasting.
Cushing’s Syndrome: Excess cortisol production can lead to muscle weakness and reduced bone density.
Cancer and Cancer Treatments: Certain types of cancer and treatments like chemotherapy can impact bone and muscle health.
Eating Disorders (such as Anorexia Nervosa): Can lead to malnutrition, affecting both bone density and muscle mass.
Multiple Sclerosis (MS): Affects the central nervous system, leading to muscle weakness and coordination problems.
Muscular Dystrophies: A group of genetic diseases causing muscle weakness and loss of muscle mass.
Vitamin D Deficiency: Essential for bone health; its deficiency can lead to weakened bones.
Parathyroid Disorders: Can affect calcium levels in the body, impacting bones and muscles.
Endocrine disorders: Hyperparathyroidism and hyperthyroidism affecting hormones
Inflammatory Bowel Diseases (Crohn’s & Colitis)
Haematological Disorders: blood diseases like anaemia, leukemia, myeloma, lymphoma, haemophilia)
Acute and Chronic Diarrhea: Causing nutritional deficiency if affected long term,
Respiratory Diseases: (COPD) Chronic Obstructive Pulmonary Disease
Lupus: a chronic autoimmune disease-causing inflammation which also impacts bone and muscle health
Parkinson’s: Individuals are at a higher risk for osteoporosis and fractures.
SIBO: (Small Intestinal Bacterial Overgrowth) where excessive bacteria grow in the small intestine and symptoms including poor nutrient malabsorption.
These conditions vary in their impact on bone and muscle health, and management may require a combination of medication, lifestyle changes, and dietary adjustments.
Medications: A Double-Edged Sword
Certain medications can detrimentally affect bone and muscle health and increase the risk of developing osteoporosis:
Corticosteroids: Long-term use can lead to bone loss and muscle weakness – steroid tablets, prednisolone, prednisone, dexamethasone.
Proton Pump Inhibitors (PPIs): Used for acid reflux, long-term use can interfere with calcium absorption – Losec, Nexium, Somac, Zoton and Pariet.
Anticonvulsants: used for epilepsy, can disrupt bone metabolism.
Certain Antidepressants – such as selective serotonin reuptake inhibitors – SSRIs, may affect bone density.
Aromatase Inhibitors: used in breast cancer treatment, can lead to bone loss.
Gonadotropin-Releasing Hormone (GnRH) Agonists: Used for conditions like prostate cancer, can affect bone density.
Glucocorticoids: Used for a variety of conditions, can lead to reduced bone formation and muscle weakness.
Thiazolidinediones: used for diabetes, can cause bone loss.
Loop Diuretics: Long-term use can lead to calcium loss from bones – furosemide
Androgen Deprivation Therapy (used for prostate cancer): Can reduce bone density.
Methotrexate (used for rheumatoid arthritis and other conditions): Can impact bone health with prolonged use.
Antipsychotics: Some can have an adverse effect on bone density.
Lithium (used for bipolar disorder): Can affect calcium metabolism and bone health.
Progestin Contraceptives: progestin-only contraceptives, particularly injectable forms like Depo-Provera can affect bone health. They decrease bone mineral density due to their impact on estrogen levels leading to decreased calcium incorporation into bone, increasing osteoporosis and fractures risks, especially with long-term use.
It’s important to note that while these medications can affect bone and muscle health, they are often necessary for managing specific medical conditions. Patients should consult with healthcare professionals to understand the risks and benefits and explore possible alternatives or mitigating strategies.
Menopause and Bone Density
During perimenopause, menopause, and post menopause, women experience significant bone density loss due to declining estrogen levels. This process typically begins in the perimenopausal phase, which can start several years before menopause (the point when a woman has not had a menstrual period for 12 months).
Perimenopause: Women may start to lose bone density at a faster rate during perimenopause, but the loss is usually more pronounced after menopause.
Menopause: The most significant bone loss occurs in the first few years after menopause, with an average loss of 2% to 6% per year. This accelerated phase of bone loss is linked to the sharp decline in estrogen production.
Post menopause: After the initial few years post-menopause, the rate of bone loss tends to slow down but continues at a rate higher than before menopause. The total bone loss during the first 5 to 10 years of menopause can be as high as 20%.
Andropause in Men
Andropause, often referred to as male menopause, affects men over about age 70 due to a gradual decline in testosterone levels which can significantly impact bone health due to altered bone remodeling and reduced muscle strength.
High Alcohol Intake
Alcohol consumption hinders osteoblasts, the cells responsible for new bone formation, leading to reduced bone production and repair. It also impairs calcium absorption and the liver’s conversion of Vitamin D to its active form, crucial for calcium uptake. Chronic alcohol use disrupts hormonal balance, increasing bone loss, and can cause liver disease, further deteriorating bone density and quality.
Cigarette Smoking
Smoking effect blood flow and metabolic health, interfering with the delivery of nutrients and oxygen necessary for bone health. Smoking decreases the absorption of calcium, disrupts hormones, reduces bone formation, increases bone resorption, and delays bone repair and fracture healing. Nicotine acts as a stimulant and has several effects on the body that contribute to reduced appetite, which may lead to nutritional deficiency, which also impairs bone health.
Vaping & Bone health
Ingesting glycol vapor, commonly found in e-cigarettes or vapes, may have potential effects on bone and metabolic health, although research in this area is still evolving. Propylene glycol and vegetable glycerine are primary ingredients in vape liquids. While these compounds are generally recognised as safe for ingestion and topical use, the long-term effects of inhaling them in vapor form are not fully understood.
Bone Health: There is emerging evidence suggesting that vaping may impact bone health. Nicotine, often present in vaping liquids, is known to affect bone density negatively. It can inhibit the function of osteoblasts (bone-forming cells) and promote osteoclasts (cells that break down bone), potentially leading to weakened bones and increased risk of fractures.
Metabolic Health: The effects of vaping on metabolic health are also under study. Nicotine can influence insulin sensitivity and might contribute to metabolic syndrome. However, specific effects attributable to glycol vapours themselves are less clear.
It’s important to note that vaping is a relatively new phenomenon, and many of the long-term health effects are still being researched. The impact on bone and metabolic health may vary depending on factors like the presence of nicotine, frequency of use, and individual health conditions. For conclusive insights, more comprehensive and long-term studies are needed.
Long Term Bed Rest
Bones and muscles adapt to the forces applied to them. Prolonged bed rest eliminates these stresses leading to a decrease in bone density and strength. Lack of exposure to sunlight (Vitamin D), impaired circulation, lower Calcium absorption, hormonal changes and reduced muscle forces on bones associated with prolonged inactivity all negatively impact on bone health.
Obesity
Obesity can lead to chronic inflammation, hormonal imbalances, Vitamin B deficiency, and a sedentary lifestyle, all of which, along with impaired mobility and metabolic syndrome, adversely affect bone health. These issues can worsen with secondary conditions like type 2 diabetes and cardiovascular diseases, further impacting bone remodelling and overall bone health.
Final Thoughts: A Comprehensive Approach
Addressing bone health requires an integrated approach, considering genetics, nutrition, lifestyle, and medical history. It’s about finding a balance and integrating strategies that work for you. Remember, maintaining strong bones is not just about preventing diseases but also about ensuring you live your best life for longer.